What are Complex PTSD Symptoms? Understanding Single Event PTSD vs. Complex Trauma in Childhood and Adolescence
Understanding Single Event PTSD vs. Complex Trauma in Childhood and Adolescence
Author: Alex Penrod, MS, LPC, LCDC
Trauma can significantly impact mental health, but not all trauma is the same. There are key differences between single event PTSD and complex trauma, especially when the latter occurs in childhood and adolescence. Understanding these distinctions and the appropriate treatment strategies is crucial for effective therapy. In this article, we will delve into the nuances of single event PTSD and complex trauma and explore psychologist Pierre Janet's 3-phase model of trauma recovery.
What is Single Event PTSD?
Single event PTSD typically arises from a one-time traumatic event, such as a car accident, natural disaster, or violent assault. The symptoms can include flashbacks, nightmares, severe anxiety, and uncontrollable thoughts about the event. While debilitating, treatment for single event PTSD can be relatively straightforward with evidence-based therapies like Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR).
Understanding Complex Trauma
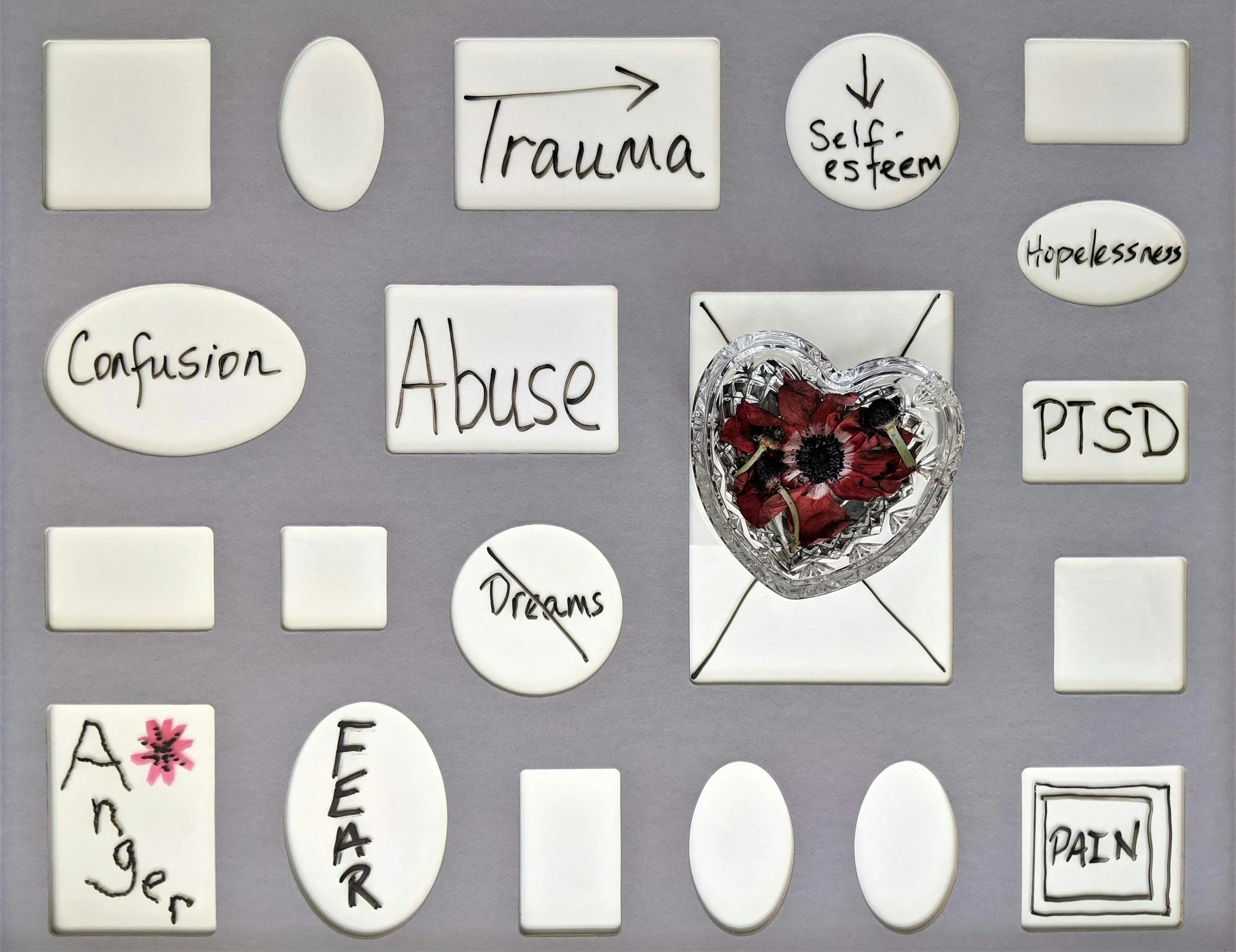
Complex trauma, recently defined as the diagnosis of complex PTSD (C-PTSD), typically results from prolonged or repeated exposure to traumatic events, often occurring during childhood and adolescence. This can include abuse, neglect, domestic violence, or other persistent stressors. Complex trauma deeply affects a child's development and can lead to profound emotional and psychological difficulties that persist into adulthood.
Differences Between Single Event PTSD and Complex Trauma
Nature of Trauma:
Single Event PTSD: Arises from a single, isolated traumatic incident.
Complex Trauma: Stems from ongoing, repetitive traumatic experiences, often starting in childhood. Diagnosis is based on symptoms and having multiple or ongoing traumatic events in one’s history is not a requirement.
Symptoms:
Single Event PTSD: According to the Diagnostic and Statistical Manual of Mental Disorders (DSM)-5-TR, to be diagnosed with PTSD, a person needs to have experienced the following symptoms for a duration greater than one month:
At least one re-experiencing or intrusion symptom:
Recurrent, involuntary, and intrusive distressing memories of the traumatic event(s)
Recurrent distressing dreams in which the content and/or affect of the dream are related to the traumatic event(s)
Dissociative reactions (e.g., flashbacks) in which the individual feels or acts as if the traumatic event(s) were recurring.
Intense or prolonged psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event(s).
Marked physiological reactions to internal or external cues that symbolize or resemble an aspect of the traumatic event(s).
At least one avoidance symptom beginning after the event(s):
Avoidance of or efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s).
Avoidance of or efforts to avoid external reminders (people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s).
Negative alterations in cognition and mood beginning or worsening after the event in the form of two (or more) of the following:
Inability to remember an important aspect of the traumatic event(s) (typically due to dissociative amnesia, and not to other factors such as head injury, alcohol, or drugs).
Persistent and exaggerated negative beliefs or expectations about oneself, others, or the world (e.g., “I am bad,” “No one can be trusted,” “The world is completely dangerous”).
Persistent, distorted cognitions about the cause or consequences of the traumatic event(s) that lead the individual to blame himself/herself or others.
Persistent negative emotional state (e.g., fear, horror, anger, guilt, or shame).
Markedly diminished interest or participation in significant activities.
Feelings of detachment or estrangement from others.
Persistent inability to experience positive emotions (e.g., inability to experience happiness, satisfaction, or loving feelings).
Marked alterations in arousal and reactivity associated with the traumatic event(s), beginning or worsening after the traumatic event(s) occurred, in the form of two (or more) of the following:
Irritable behavior and angry outbursts (with little or no provocation), typically expressed as verbal or physical aggression toward people or objects.
Reckless or self-destructive behavior.
Hypervigilance.
Exaggerated startle response.
Problems with concentration.
Sleep disturbance (e.g., difficulty falling or staying asleep or restless sleep).
In addition, PTSD may involve dissociative symptoms, including:
Depersonalization: Persistent or recurrent experiences of feeling detached from, and as if one were an outside observer of, one’s mental processes or body (e.g., feeling as though one were in a dream; feeling a sense of unreality of self or body or of time moving slowly).
Derealization: Persistent or recurrent experiences of unreality of surroundings (e.g., the world around the individual is experienced as unreal, dreamlike, distant, or distorted).
Complex Trauma (C-PTSD): According to the World Health Organization, C-PTSD requires all the criteria for a diagnosis of PTSD to be met, plus at least one symptom from each of the Disturbances of Self-Organization categories:
Affect dysregulation:
Severe difficulty and taking a long time to feel calm again after being emotionally upset.
Feeling emotionally numb or shut-down.
Negative self-concept:
Feeling like a failure
Feeling worthless
Disturbances in relationships
Feeling distant or cut-off from people
Finding it hard to stay emotionally close to people
Impact on Development:
Single Event PTSD: May not significantly disrupt developmental milestones.
Complex Trauma (C-PTSD): Can severely impact developmental processes, including attachment, self-regulation, and cognitive functioning.
Treatment Approach
Single Event PTSD: Responds well to evidenced based treatments such as TF-CBT and EMDR alone without much modification.
Complex Trauma (C-PTSD): Often requires extended preparation for memory reprocessing therapies, modifications to protocols, and/or a phased approach outlined below.
Considerations on Diagnosis and Categorizing Trauma
The fight for C-PTSD to be an official diagnosis has been a multi-decade struggle pioneered by experts such as Dr. Judith Herman, who released her seminal book, Trauma and Recovery, outlining C-PTSD in 1992. It took another 30 years for C-PTSD to be included in the ICD-11 codes, effective January 1, 2022. The following is my clinical opinion and should be taken as an opinion. The diagnosis of traumatic responses (single event and complex) has historically stirred controversy and debate as to whether these responses are real, what qualifies as a traumatic event, where the bar should be set for diagnosis, and how it should be treated. Historically, the survivors of trauma have had to endure invalidation, dismissal, misdiagnosis, and ineffective or inadequate treatments while the “experts” have debated on how to categorize and deem trauma worthy of being treated. This has resulted in much undeserved and unnecessary pain and suffering for trauma survivors.
For the purposes of research and insurance reimbursement, diagnosis is a critical aspect of treatment. For the purpose of identifying, validating, and alleviating human suffering, in my opinion a person does not need to meet full criteria for a diagnosis to be in need of and benefit from trauma therapy. A careful and thoughtful assessment should be made to determine how to best match the type of therapeutic approach to the person’s needs, symptoms, and goals. I view therapy as a holistic endeavor that should validate and honor the lived experience of a person and assist in them achieving their personal goals for therapy, whether they fall nicely into a diagnostic category or somewhere in between.
Treatment Strategies for Complex Trauma
C-PTSD often requires a more nuanced and comprehensive approach that goes beyond the methods used for single event PTSD. Janet's 3-phase model of trauma recovery provides an effective framework for treating complex trauma, and has been recommended for several decades. Multiple evidence based treatment methods, coping strategies, and non-clinical resources can be woven into the following phases as needed.
Phase 1: Stabilization
Focus: Establishing safety and stability in daily life.
Techniques: Developing coping skills, establishing routines, finding a safe environment, and fostering a sense of control over one’s emotions and nervous system.
Therapies: Dialectical Behavior Therapy (DBT), Ego State Therapy, Internal Family Systems Therapy (IFS), Somatic Experiencing (SE), grounding techniques, breathing techniques, embodied movement like yoga, and mindfulness practices.
Safety involves having people and an environment that aren’t posing a constant threat. Stabilization involves regaining a sense of safety and control over one’s body and emotions when faced with triggers or reminders of threat. Phase 1 can last weeks, months, or years, and some people find no need to work with trauma memories once they feel stabilized. During this phase I provide a lot of education, work to build trust with you, help you practice regulation strategies in real time, and introduce you to ego state therapies.
Phase 2: Memory Reprocessing
Focus: Activating and processing traumatic memories at a pace and quantity the individual can tolerate.
Techniques: Gradual exposure to traumatic memories, cognitive restructuring, and emotional processing.
Therapies: Eye Movement Desensitization and Reprocessing Therapy (EMDR), Trauma-Focused Cognitive Behavioral Therapy (TF-CBT), Prolonged Exposure Therapy (PE). The unburdening phase of IFS can be used as well.
For phase 2 I specialize in EMDR. However, the goal of each therapy listed above is to move the memories from an unprocessed disturbing state to an integrated and neutral state. Many people find after reprocessing traumatic memories their triggers reduce in frequency and intensity or go away, they have less intrusive thoughts, their nightmares reduce or stop, and they are spending much less energy on avoiding and repressing their internal experiences. For more information on how EMDR accomplishes this, check out my blog on the neuroscience behind EMDR here. Memory reprocessing paves the way for phase 3 which involves building intentional and self-affirming structures in the void that was previously occupied with trauma symptoms and managing life around them.
Phase 3: Reintegration and Rehabilitation
Focus: Building a future and integrating the trauma into one's life narrative.
Techniques: Enhancing life skills, fostering healthy relationships, developing a sense of identity and purpose.
Therapies: Narrative therapy, life coaching, vocational training.
Living with the lasting effects of trauma can be isolating, limiting, and puts constraints on the development of the personality. When you begin to heal and feel a greater sense of confidence the opportunities for growth can be exciting while also a new source of overwhelm. When your brain begins to view life as something to explore rather than brace yourself against, the work shifts to experimenting with this new territory while maintaining the stability built in the previous phases. Phase 3 is centered around the concept of post traumatic growth. In this sense, you are not returning to a previous state, but becoming more of who you intentionally want to be. Because C-PTSD often involves childhood trauma, the reintegration phase can offer an open window for the development or revision of personal identity, one that is more chosen and feels positive and empowering. This could manifest as new hobbies, career opportunities, relationships, or unexpected discoveries about yourself. Seeing my clients in this phase of their process is one of the most rewarding parts of my work.
Discussion
Complex trauma may be complex, but the guidelines for treatment may rival its complexity. Previous guidelines from the International Society of Traumatic Stress Studies (ISTSS) recommended a 3-phased approach to treatment for C-PTSD, however recent research has started to show that completing an initial “stabilization” phase shows no superiority over immediately focusing on processing traumatic memories. Further, there has been much debate around what exactly constitutes the "reintegration” of phase 3 of Janet’s model, making it difficult to research or prove it is necessary. ISTSS currently recommends an individualized approach in which there is no push to follow a rigid protocol, the best practice is to custom tailor therapy to the needs and presenting symptoms of the individual. This seems level headed and reasonable considering the new research shows that allowing clients to stabilize prior to memory reprocessing is no less effective than immediately focusing on traumatic memories. My clinical experience shows me that stabilization is typically necessary, as C-PTSD often involves symptoms of dissociation or a co-occurring dissociative disorder (a topic I will cover in a separate blog). The guidelines for the use of EMDR therapy with clients who dissociate firmly recommend an extended preparation period prior to memory reprocessing.
As such, although I work within the 3-phase model as my orientation, how quickly you move through each phase or whether you need to spend much time in each phase depends entirely on your needs and the collaboration between us to determine where to go next. Ultimately, you are in control of your therapy and you’re free to make your own choices based on the education I provide. I support your judgment about what you can or cannot tolerate or how fast to move, and there are ways to gauge your tolerance and readiness for memory reprocessing without diving into the deep end of the pool.
Conclusion
Understanding the differences between single event PTSD and C-PTSD is essential for effective treatment. While single event PTSD often responds well to targeted interventions like CBT and EMDR alone, C-PTSD often requires a more comprehensive phased approach. EMDR can be adapted and integrated into the overall treatment strategy seamlessly. Having a definite answer on exactly what to do and when to do it in therapy would be wonderful, but the clue as to why this is elusive is in the name - complex trauma. In the absence of clear and overwhelming consensus among the experts, working with a thoughtful, experienced, and well-trained therapist can allow you the flexibility to find the solutions that work best for you, and isn’t that what really matters?
Alex Penrod, MS, LPC, LCDC
August 5th, 2024
References
American Psychiatric Association. (2022, November). What is posttraumatic stress disorder (PTSD)?. Psychiatry.org. https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd
Brewin, C. R. (2019, August 8). Complex post-traumatic stress disorder: A new diagnosis in ICD-11: Bjpsych advances. Cambridge Core. https://www.cambridge.org/core/journals/bjpsych-advances/article/complex-posttraumatic-stress-disorder-a-new-diagnosis-in-icd11/2977140CBDAAF402610715BB609F688C
Condon, M., Bloomfield, M. A. P., Nicholls, H., & Billings, J. (2023). Expert international trauma clinicians’ views on the definition, composition and delivery of reintegration interventions for complex PTSD. European Journal of Psychotraumatology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9848321/
Jongh, A. de, Bicanic, I., Matthijssen, S., Amann, B. L., Hofmann, A., Farrell, D., Lee, C. W., & Maxfield, L. (2019, November 1). The current status of EMDR therapy involving the treatment of complex posttraumatic stress disorder. Journal of EMDR Practice and Research. https://connect.springerpub.com/content/sgremdr/13/4/284
Sussex Publishers. (2024). Judith L. Herman M.D. Psychology Today. https://www.psychologytoday.com/us/contributors/judith-l-herman-md
van der Hart, O., Brown, P., & van der Kolk, B. (1989). Janet’s treatment of post-traumatic stress. Journal of Traumatic Stress. 2(4):379-395. https://www.researchgate.net/publication/226134094_Janet’s_treatment_of_post-traumatic_Stress
van Vliet, N. I., Huntjens, R. J. C., van Dijk, M. K., Bachrach, N., Meewisse, M.-L., & de Jongh, A. (2021, November 16). Phase-based treatment versus immediate trauma-focused treatment for post-traumatic stress disorder due to childhood abuse: Randomised clinical trial. BJPsych Open. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8612023/